A Pediatric Surgeon’s Perspective on Advancing Surgical Care for Children with Cancer in Latvia
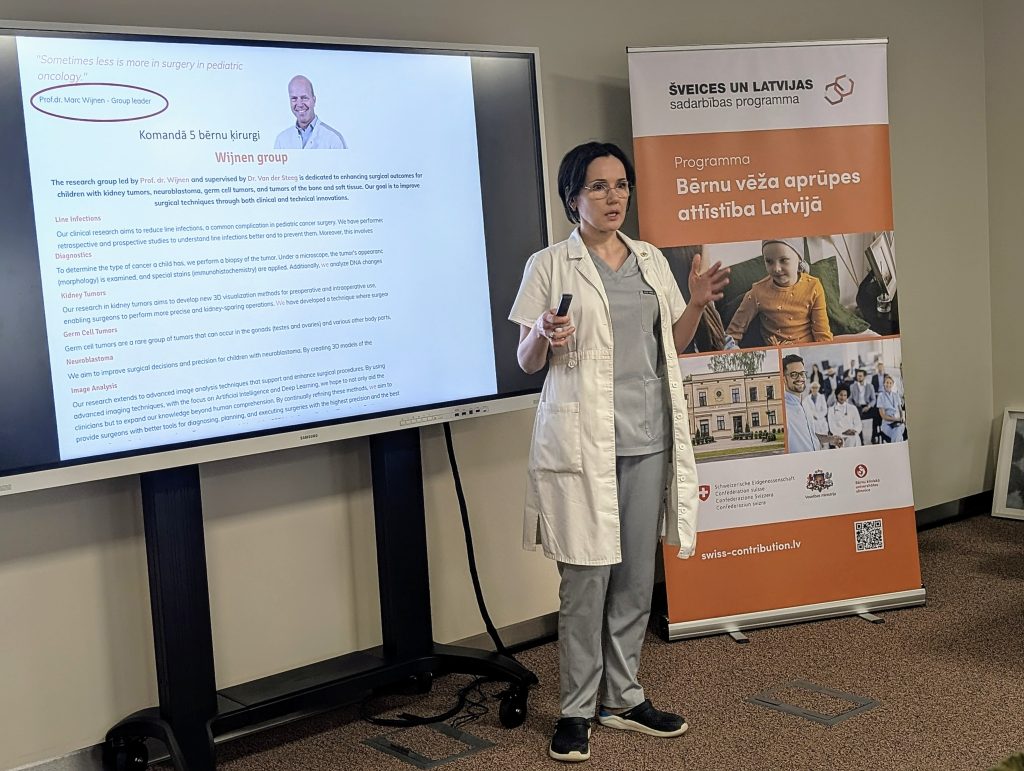
As part of the Swiss–Latvian Cooperation Programme “Advancement of Paediatric Cancer Care in Latvia”, Dr. Zane Ābola, Head Surgeon at the Children’s Surgery Clinic of the Children’s Clinical University Hospital (CCUH), spent February 2025 on a professional exchange visit at one of Europe’s leading paediatric oncology centres. Her destination, the Princess Máxima Centre for Paediatric Oncology in Utrecht, the Netherlands, was chosen for its extensive experience in treating rare and complex cancer cases in children. Upon her return to CCUH, Dr. Ābola shared her insights at a knowledge-sharing event titled “What is a Modern Approach to Paediatric Oncology – A Surgeon’s Perspective.”
“These kinds of international projects, like the Swiss–Latvian programme, are extremely important as they offer physicians from different specialties the opportunity to learn from colleagues abroad and adopt best practices. Modern medicine cannot develop in isolation – we need fresh perspectives to reflect on what we do and how we do it, and to be inspired by alternative approaches.
While the Swiss–Latvian cooperation programme offers many benefits, the most valuable aspect for me as a surgeon working with paediatric oncology patients is the opportunity to build sustained collaboration with international colleagues – especially in finding the most effective ways for oncologists, surgeons, and other specialists to work together in daily practice,” said Dr. Ābola.
Latvia is a relatively small country, and the number of paediatric cancer cases is comparatively low. For medical professionals, this means fewer opportunities to gain experience with the most complex cases. The exposure gained from working at one of Europe’s leading centres—where patients come not only from the Netherlands but from abroad—provided unique insights into highly effective and evidence-based treatment approaches. If necessary, children from Latvia can already be referred for treatment abroad, but it is vital to continue building strong partnerships with other countries.
At the Princess Máxima Centre, the number of trainees is carefully managed to ensure high-quality learning for everyone. Dr. Ābola had the opportunity to observe international teams, participate in surgical procedures, and engage in multidisciplinary tumour board meetings. Special attention was paid to patient experience and safety.
One key observation was how surgical teams are structured. In Latvia, paediatric surgeons also handle emergency cases, while at the Princess Máxima Centre, surgeons are fully specialised in oncology. Scientific research is also an integral part of their daily work – something Latvia should increasingly aim for.
What left the greatest impression on Dr. Ābola was the centre’s focus on personalised care – a key principle of precision medicine, which is also gaining ground in Latvia. At the Princess Máxima Centre, this is a clearly defined practice. For example, when a biopsy is performed on a patient with a suspected malignant tumour, a lab technician is present in the operating room to perform immediate microscopic analysis. The specimen is later sent for further detailed laboratory analysis, including genetic testing – part of which is already performed in Latvia. While we are making progress, there are specific practices we can adopt to enable more precise intraoperative decision-making.
Precision medicine is closely linked to research. Today’s oncology projects, which increasingly involve surgeons, offer opportunities to significantly improve care quality. One such innovation is the use of 3D tumour models. Before surgery, these patient-specific models provide a detailed, physical representation of the tumour’s size, location, and proximity to blood vessels and organs. This enables the surgeon to plan the procedure more accurately, especially in cases where tumour placement is atypical.
While 3D modelling is not new to Latvia, it is not yet a routine part of clinical practice. There is no established system or protocol for regular use, and funding models are unclear. Developing a sustainable framework for integrating these technologies into standard treatment pathways is still needed.
The “Advancement of Paediatric Cancer Care in Latvia” programme is funded by Switzerland and aims to improve diagnostics, treatment, and the quality of life for children with cancer or rare diseases, ensuring a continuum of care with a patient-centred, multidisciplinary approach.
Read more



