CCUH Strengthens Infection Control for Paediatric Oncology Patients
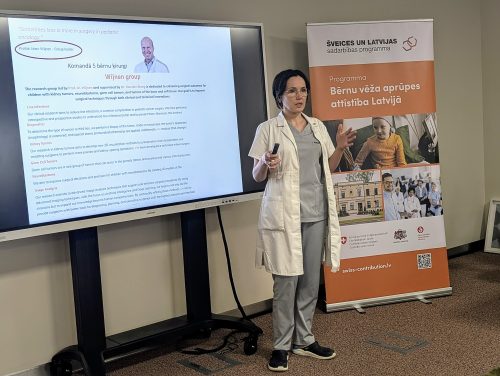
The opportunity for specialists from the Children’s Clinical University Hospital (CCUH) to engage in knowledge exchange and training at leading paediatric oncology centres across Europe is improving the quality of care and treatment for patients in the hospital’s Haemato-Oncology Department. Within the framework of the Swiss–Latvian Cooperation Programme “Advancement of Paediatric Oncology Care in Latvia”, one key focus — relevant globally — is the implementation of targeted measures to reduce the risk of invasive fungal infections during cancer treatment. In close collaboration with leading international experts, paediatrician and infectious disease specialist Dr. Liene Smane is applying global best practices at CCUH.
Dr. Liene Smane explains:
“Children undergoing treatment for cancer face challenges not only from the disease itself but also from serious treatment-related side effects. Cancer therapy severely weakens the immune system, making children more vulnerable to life-threatening infections, including invasive fungal infections. Some patients, due to specific diagnoses, receive more intensive treatment and are therefore at higher risk of fungal complications. For these patients, it is crucial to start antifungal prophylaxis simultaneously with cancer therapy.
There are cases where a child does not die from their underlying haemato-oncological disease, but from an invasive fungal infection that develops during treatment. By following international recommendations for antifungal prophylaxis, we can offer children more effective protection against these serious infections, significantly improving survival rates, reducing complications, and ensuring safer, higher-quality care.”
However, prophylactic therapy itself may have side effects and interact with cancer medications. Therefore, treatment choices must be based on evidence from international research, tailored to each individual case. Latvia, as a small country, has limited national data, which is why cooperation and knowledge exchange with international centres is essential.
“Thanks to the Swiss–Latvian Cooperation Programme, I have been able to build contacts and learn directly from leading experts in Swiss hospitals, attend international conferences, specialised trainings, and networking events. Even after returning from my visits, I continue consulting top specialists in paediatric oncology who treat the most complex cases and see patients from around the world daily,” says Dr. Smane.
Antifungal prophylaxis is already a standard part of care in CCUH’s Haemato-Oncology Department, but it is essential to stay updated with the latest research. Going forward, CCUH plans to establish a multidisciplinary approach to infection prevention, involving haemato-oncologists, infectious disease specialists, pharmacists, and laboratory professionals. When introducing new medications, it is vital to understand their pharmacokinetics, pharmacodynamics, and drug interactions — all of which require a collaborative team approach. Each case must be assessed individually, and the effectiveness of prophylactic treatment must be monitored through measurable outcomes. This aligns with the global shift toward personalised medicine in paediatric oncology.
“When we choose both the most effective primary treatment and preventive therapy, we not only achieve better outcomes but also ensure that treatment is not interrupted due to serious infections. For patients and their families, this means shorter hospital stays and fewer emotional and physical burdens. Avoiding severe infections significantly improves the quality of life during and after treatment,” Dr. Smane adds.
Education also plays a critical role. Children respond better to infection prevention when they and their families follow special dietary recommendations, known as a neutropenic diet. During the NOPHO-NOBOS congress, one of the leading events in paediatric oncology in the Nordic and Baltic regions, Dr. Smane became familiar with the latest evidence-based nutritional guidelines. Together with colleagues, she has developed educational materials for families of children with cancer and provides counselling to support adherence to treatment protocols.
“Only with strong collaboration between healthcare professionals, children, and families can we achieve the best possible treatment outcomes,” says Dr. Smane.
The “Advancement of Paediatric Oncology Care in Latvia” programme is implemented with financial support from Switzerland. Its goal is to improve diagnosis, treatment, and quality of life for children affected by cancer or rare diseases, while ensuring continuous, patient-centred care.

Read more